21 February 2018
In the second blog of our Value Based Healthcare series Professor John Moxham blogs about why better outcomes drive better value.
In my first blog on 25 January I set out the view that it is only by focusing on increasing value in health and healthcare that sustainable high-quality care can be delivered to our patients and population. We defined value as outcomes that matter to patients, service users and carers, over the costs of achieving those outcomes, over the complete pathway of care.
I pointed out it is crucial to focus on (and document) outcomes that matter to patients and gave the example of stroke. Patients who have strokes want to survive, but they also want a full recovery, as quickly as possible, without complications, and do not want a recurrence.
Watch Professor Moxham's short video on patient outcomes, part one of our Value Based Healthcare miniseries:
At King’s Health Partners our approach to Value Based Healthcare is set out in our strategy and is much influenced by the writings of Michael Porter and colleagues at Harvard. Our lens on outcomes reflects Porter’s hierarchy, as set out below:
- Health status achieved (survival and degree of recovery)
- Process of recovery (time to recovery and return to normal activities, disutility of care or treatments – quality of care measures e.g. diagnostic errors, unsafe care, ineffective care, over investigation and treatment, complications)
- Sustainability of health (sustainability of recovery, nature of recurrences, long-term adverse consequences of therapy).
It is clear that these outcomes reflect the sum of all activities across complete pathways of care, often delivered by multiple care providers. The stroke pathway for example can include care from ambulance services, hospitals, rehabilitation services, primary care, social care, and families. Furthermore, many conditions, including most strokes, are caused by disease processes that can be considered to constitute the front end of the pathway (e.g. for stroke - vascular disease secondary to smoking, diabetes, hypertension).
Indeed for some pathways the strongest value proposition can be prevention rather than treatment. Reflecting this at King’s Health Partners we are trying to reduce the burdens of alcohol and smoking in our populations through our alcohol and tobacco strategies.
Given the importance of measuring outcomes that matter to patients and carers it is surprising that such measurements are often not made. They are rarely collected systematically, documented, published, or shared with staff.
A major problem is that if members of a particular healthcare team are not collecting, or are not aware of the outcomes that their efforts are producing, how can they know how good a job they are doing? How can they know if they are doing better this year than last, or whether any changes they have made, or been required to make to their services have improved the lives of their patients?

[Image: This graph shows improvement of Health of the Nation Outcome Scores (HoNOS) following treatment from perinatal services at the Mother and Baby Unit at South London and Maudsley. Read the Psychological Medicine CAG Outcomes Book for more information.]
Thus, for many reasons, King’s Health Partners regards the measurement and sharing of outcomes as essential and we are asking all of our 22 Clinical Academic Groups (CAGs), which collectively cover all the clinical services of our Academic Health Sciences Centre, to publish Outcomes Books.
Our CAG Outcomes Books are published on our website and to date we have posted 11 books, with two more to be added before April 2018. Additional books will follow shortly thereafter.
Although we expect the books to be helpful to an external audience, including commissioners of services and our patients and carers, we believe that their impact on our own staff is particularly important. We believe that our staff have a right, and even a duty, to see the outcomes of their work presented in a clear and engaging format. We would concur with Michael Porter (Harvard) when he says:
“It is nice to compare yourself to others; the really important thing is to show how you are doing year on year.”
Similarly we agree with Toby Cosgrove (Cleveland Clinic Chief Executive Officer for 13 years) who said:
“Although it is important to share outcomes with patients and the public, the main benefit is that it holds up a mirror to the organisation and tells the Clinic and the Institutes how well they are doing and whether or not they are improving”.
The Cleveland Clinic has a long history of publishing outcomes and in this regard King’s Health Partners is enthusiastically seeking to follow their example.
As the NHS seeks to maintain and improve the care of millions of patients, despite the unprecedented constraints on resources, enhancing the performance of clinical teams is of fundamental importance. The feedback of outcomes data to staff, not confined to process metrics but including outcomes that matter to patients, is essential to drive improvement. Without feeding back to staff, the cultural change necessary to drive improvements in outcomes will not occur. We all know that the vast majority of our staff want to do the very best they can for their patients. They have a right to know the outcomes they are achieving.
It is of interest that analysis of the results of the inspections by the Care Quality Commission (CQC) of all healthcare providers in England has demonstrated that the single measure that best correlates with the CQC assessment results is whether clinical staff believed they were able to deliver good outcomes to patients. There can be little doubt that sharing data on outcomes that matter to patients has a powerful impact on staff at all levels.
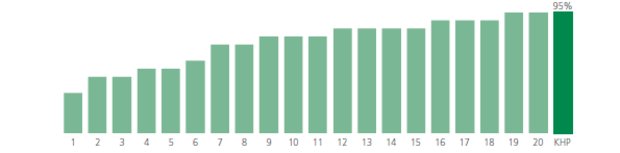
[Image: This graph shows the percentage of over 65s admitted and discharged to their usual place of residence. King's Health Partners (KHP) includes our acute trusts King's College Hospital and Guy's and St Thomas' . We discharge more patients to their usual place of residence than any other acute trust in London. For more information about the details on the graph read the Medicine CAG Outcomes Book.]
As an Academic Health Science Centre our primary goal is to integrate the tripartite agenda of clinical care, research, and education, to improve the health and wellbeing of our patients and population. Our Outcomes Books therefore report achievements in research and education as well as clinical outcomes, and also document our clinical-academic innovations that benefit patients.
Inevitably, the production of comprehensive Outcomes Books is a substantial and time-consuming task. To make core outcomes data available regularly and more quickly we are planning to produce Outcomes Scorecards and these will be the subject of a future blog.
Finally, again quoting the words of Michael Porter, we agree that “the most powerful way to drive costs down is to improve outcomes (early and correct diagnosis and treatment, fewer complications, faster and sustained recovery).”
Better outcomes drive better value.
Read more about Value Based Healthcare at King's Health Partners.