20 June 2019
We left Prof John Moxham in the early 80s with a new role at King’s College Hospital and settling into life as an enthusiastic Camberwellian. In the second part of this wide-ranging interview, our Communications Office Rachel Brooks finds out how John goes from Consultant to King’s Health Partners, embraces value, and his favourite moments from a 50-year career.
How did you go from King’s College Hospital to King’s Health Partners?
Now that I can look back - I think that my progress in medicine has been a continuous process, with each stage making the next stage possible. I have always thought that the goal of a university hospital should be to combine research, training and clinical practice. My research focused on clinical respiratory physiology and in 1990 I became a Professor of Respiratory Medicine at King’s College London. I loved bedside teaching and I was an examiner and edited a Text Book of Medicine. Clinically I led a ‘firm’ and became Chair of the Consultant Committee.
I did not plan my career but I did work hard, partly to make sure I did not fail and partly because I really enjoyed both the clinical and academic work.
[Image: John greeting Princess Ann during a royal visit]
In April 2003 I became Medical Director at King’s College Hospital, a post I held, coincidentally during the time that the hospital became clinically very strong and a Foundation Trust. I stepped down from the MD role in September 2009 after King’s Health Partners became an Academic Health Sciences Centre (AHSC) and I was appointed Director of Clinical Strategy – without the dreaded sherry round!
As an AHSC, King’s Health Partners is focused on the integration of the tripartite agenda of research, education and clinical care to improve the experience and outcomes of patients, locally, nationally and globally.
Over the years I had developed a deep understanding of the strengths in each aspect of the tripartite agenda. This helped me to deliver my responsibilities on the Executive of King's Health Partners and specifically in the role of Director of Clinical Strategy.
Much of your work for King’s Health Partners centers around improving health outcomes for patients. What motivated you to focus on this?
 Outcomes matter hugely to patients. Of course, process is important, but it is outcomes that we should be focusing on.
Outcomes matter hugely to patients. Of course, process is important, but it is outcomes that we should be focusing on.
To put it bluntly - when patients go to see doctors with a problem they want that problem addressed– that is their definition of a good outcome. But the NHS generally tends to concentrate on process and even receiving rapid treatment in wonderful facilities delivered by first class staff counts for little if the outcomes are sub-standard.
[Image: John at King's College Hospital in 2005 when he was Medical Director]
The UK is not doing well on outcomes and compared with our comparator nations we have steadily slipped down the rankings. A key question in healthcare is “Are we getting better or worse?” If we do not have accurate and comprehensive outcome measurements, we cannot answer this crucial question.
So what has King’s Health Partners been doing about that?
I wanted King’s Health Partners to lead the way in reporting and relentlessly improving outcomes. I was inspired by the outcomes books published by the Cleveland Clinic.
Outcomes are at the heart of driving better value. We define value as those outcomes that matter to patients, divided by the costs of producing those outcomes, measured over the complete pathway of care.
The key purpose of our AHSC is to integrate research, education and clinical care to improve health locally and globally. It is important that progress on this huge ambition, particularly progress in improving outcomes, is documented by our Clinical Academic Groups (CAGs) in their Outcome Books. These books provide the proof that we are delivering on our mission and I am delighted that 17 of our 22 CAGs have now published Outcome Books.
My goal is to make this 20 out of 22 before I step down and I would like to see CAGs publishing regular updates, of their outcomes across the tripartite agenda, through the use of annual scorecards.
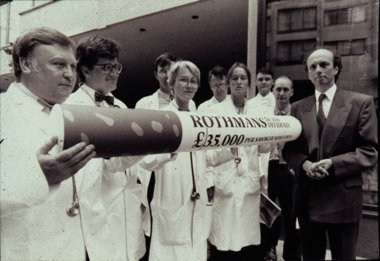
![JM capaigning for end to tobacco advertising]() You initiated the Vital 5 programme to improve outcomes for patients and our wider population – can you tell us why?
You initiated the Vital 5 programme to improve outcomes for patients and our wider population – can you tell us why?
For our adult population we know the main causes of death and disability.
If you look at the Global Burden of Disease for south east London for example, at the very top are smoking, hypertension, obesity and alcohol excess. And in terms of morbidity, depression and anxiety have become very important.
[Image: John campaigning against smoking advertising in the 1980s]
These factors are the Vital 5 and all can be easily measured. The goal is to measure the Vital 5 for each and every patient and populate a scorecard which will be shared across the healthcare system, and with the individual, to support optimal management of these five key risk factors.
Better control of raised blood pressure, obesity, smoking, alcohol excess and mental ill health in our communities would dramatically improve health outcomes, life expectancy and healthy life expectancy. If we are able to reach all adults in society, regardless of socio-economic status and ethnicity, we will greatly narrow the dreadfully wide health inequalities we currently have.
What has been the progress on the Vital 5 so far?
I am very pleased to say that the Vital 5 has received remarkable support and is being strongly endorsed by the leaders of the NHS in south east London. It is embedded in the commissioning plans of the Sustainability and Transformation Partnership (STP) and is being taken forward within King’s College Hospital and Guy’s and St Thomas’ NHS Foundation Trusts, and in Primary Care. We are also engaged in constructive talks with NHS England and Public Health England.
In the future, the mass of data made available through the Vital 5 programme will allow targeted and better interventions to improve population health. Success with the Vital 5 will gradually and progressively reduce the burden of ill health in our community, improve life and health life expectancy and make the healthcare system more financially sustainable.
The recently published NHS Long Term Plan requires the healthcare system to improve outcomes and reduce health inequalities – success with the Vital 5 programme would contribute enormously.
Your existing role is being split to help take this agenda forward - what advice would you give to those who will be taking on the cause?
We have a mantra in the Value Based Healthcare team – ‘keep on keeping on’.
 Ultimately my top piece of advice is that ownership of Value Based Healthcare and the Vital 5 does not only sit inside the hospital setting. A hospital can make a big contribution – but it’s what goes on in social and primary care and our communities that will often have the biggest impact. We can only deliver value and the Vital 5 in partnership with others. My advice to people who want to take this on is that they need to engage with everyone - communities, patients and the population, primary and community care - to change hearts and minds to get the programme integrated across the healthcare system.
Ultimately my top piece of advice is that ownership of Value Based Healthcare and the Vital 5 does not only sit inside the hospital setting. A hospital can make a big contribution – but it’s what goes on in social and primary care and our communities that will often have the biggest impact. We can only deliver value and the Vital 5 in partnership with others. My advice to people who want to take this on is that they need to engage with everyone - communities, patients and the population, primary and community care - to change hearts and minds to get the programme integrated across the healthcare system.
[Image: John and colleagues from Action on Smoking and Health, which he was formerly chair of]
This means we must ‘keep on keeping on’ consistently and continuously spreading this message every day.
What are your favourite memories at King’s Health Partners?
So many it would make an enormous list!
Any list would be topped with the people I have worked with - dozens and dozens of brilliant people who totally ‘get’ the wonderful ambition of creating a world class AHSC that benefits patients locally and globally.
I can recall many highlights in the years of forming the AHSC, particularly a wonderful group visit to Johns Hopkins University. Then there was the agreement to adopt the Clinical Academic Group structure that means we can involve all staff and students, at all levels, in the work that we do – initially this was controversial, but we prevailed.
I have always been a big believer in the integration of mental and physical healthcare through the Mind & Body programme. It is a programme that is unique to King’s Health Partners. Taking the time to ensure the provision of mental healthcare within our physical healthcare CAGs and vice versa is an ongoing process which continues to be very important to me and I will watch progress with great interest.
The inclusion of Value Based Healthcare as a cross-cutting theme in our re-accreditation application five years ago was a particular highlight. We’ve since built excellent relationships with Lambeth and Southwark Clinical Commissioning Groups, our partners in Primary Care and GPs. I had a moment of great pleasure when Lord Butler, a former Cabinet Secretary and now a Non-Executive Director, at a meeting of the King’s Health Partners Joint Boards, described the Vital 5 concept and programme as ‘pure genius’.
 I would like also to pay tribute to our leader and Executive Director Prof Sir Robert Lechler who said in 2004 that he was going to ensure we ‘punched above our weight’ – I believe he has been instrumental in helping us achieve this.
I would like also to pay tribute to our leader and Executive Director Prof Sir Robert Lechler who said in 2004 that he was going to ensure we ‘punched above our weight’ – I believe he has been instrumental in helping us achieve this.
Ultimately the whole King’s Health Partners journey has been pure magic for me.
Finally – do you have any projects or plans for your retirement?
I have four wonderful grandchildren, so I am looking forward to spending more time with them. I would of course like to continue my work at a much more local level, supporting the healthcare of my local population in Camberwell.
My wife thinks I should become a grass roots revolutionary OAP, but there will always be time for lying under trees.
[Image: John Moxham having a rest in the grass on holiday in Dieppe]



 You initiated the Vital 5 programme to improve outcomes for patients and our wider population – can you tell us why?
You initiated the Vital 5 programme to improve outcomes for patients and our wider population – can you tell us why?

