25 September 2019
As part of Sickle Cell Awareness Month, we asked Prof Jo Howard to outline how King’s Health Partners Haematology is making a difference to patients.
What is sickle cell disease?
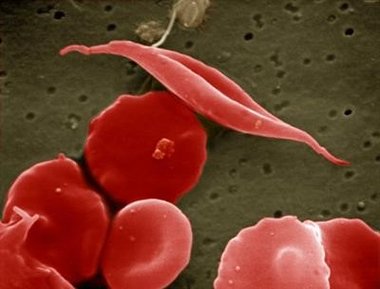
Sickle cell disease, which causes a wide range of severe and even life-threatening consequences, is caused by a single misspelling in the DNA instructions for haemoglobin, a protein vital for carrying oxygen in the blood.
As a result of this misspelling, individuals with sickle cell disease experience lifelong complications including anaemia, infections, stroke, tissue damage, organ failure, and intense painful episodes.
The disease’s debilitating symptoms and the complex treatment needs of people living with sickle cell disease often limit their education, career opportunities, and quality of life. The condition can lead to premature death.
How many patients does King’s Health Partners see with sickle cell disease?
15,000 people across England are living with sickle cell disease, and of these more than 4,000 live within the catchment for King’s Health Partners and its extended network. Based on past trends, we expect the numbers of patients we see with sickle cell disease to grow significantly in the coming years.
What are the challenges of treating people with sickle cell disease?
There are a number of challenges when it comes to treating people with sickle cell disease and as health professionals we have much more we can be doing.
Sickle cell disease is a long-term condition that requires complex management. We must be confident and skilled in educating patients on how they can manage the condition, pain management crises, and any co-morbidities.
This is particularly true for children and young people living with sickle cell disease. Many children with sickle cell disease do not receive the essential investigations which allow early identification of potential serious complications from the disease and early treatment to prevent these.
A major issue is equality of access to treatments, including pain relief for treatment of acute crisis. There is also limited access to new and experimental treatments taking place, such as automated red cell transfusion therapy and hydroxycarbamide (also known as hydroxyurea) therapy, which is the only currently licensed drug treatment for sickle cell disease. Improving access to new treatment methods and therapies – as well as optimising existing treatments and pathways – will make a difference.
Improving staff awareness outside of specialist services is vital, particularly in A&E. As an example, we know that people with sickle cell disease in emergency departments experience longer delays to administration of pain relief medication compared with other patients. We also need to examine the community support that patients receive when they leave hospital to ensure continuity of high-quality care.
We need more high-quality research to identify predictors of the severity of the disease and to improve outcomes for patients.
How has King’s Health Partners Haematology been making a difference to patients with sickle cell disease?
King’s Health Partners Haematology provides clinical leadership for sickle cell disease locally. We’re part of the South Thames Sickle Cell and Thalassaemia Network, which was founded in 2011 and involves 10 trusts, caring for more than 4,000 patients with sickle cell disease. As part of this network we host monthly multidisciplinary meetings where all local clinicians can phone in to discuss complex cases.
We also work closely with colleagues from other specialities to offer a large range of multiprofessional clinics which have allowed us to build up unique expertise in management of chronic sickle complications. Our doctors and nurses regularly speak at meetings across the network to provide education for general paediatric and haematological clinical staff.
Beyond our immediate locality, our lead consultants regularly contribute in developing national guidelines, including the recently published standards for the clinical care of adults with sickle cell disease. Our staff are also regularly invited to speak at national and international meetings.
We provide outreach specialist clinics across the network aiming to see every patient with sickle cell disease at least once a year. Patient support meetings are organised regularly and advertised across the network, including a Christmas party, an annual patient education meeting and Tree of Life meetings to provide support for teenagers.
How are you incorporating Mind & Body principles?
The mind and body are inseparable, and mental and physical health conditions are intrinsically connected. For more than 20 years we have run an integrated health psychology service. This is now a well-established service for our patients. Psychology staff participate in our inpatient ward rounds and in our outpatient clinics aiming to see all patients at least annually, and more frequently if needed.
What’s next for the Institute’s work on sickle cell disease?
We have the largest sickle research portfolio in the UK and offer patients the opportunity to participate in clinical trials with new drug treatments. We were highly rated in recent peer reviews and are exemplars in audited performance in relation to hydroxycarbamide use, acute chest condition and pain management.
Our major aim is to be able to offer curative treatments such as haematopoietic stem cell transplantation and gene therapy within the next year.
King’s Health Partners Haematology is aiming to bring together our strengths in clinical service, research, and education to deliver exceptional outcomes for haematology patients. Our vision is to develop cures and vaccinations for haematological conditions so that future generations do not have to face lives with these diseases.