2 March 2022
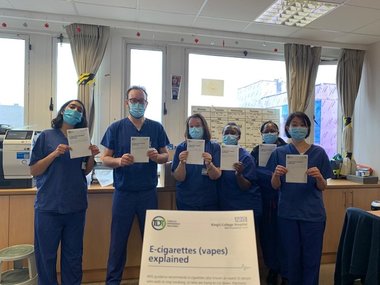
Ahead of No Smoking Day on 9 March 2022, our Events Officer, Wenda Aitchison, caught up with Arran Woodhouse* (pictured, 2nd from the left) to find out more about the Tobacco Dependence Treatment project. The photo on the right shows the Tobacco Dependence Team when they received the first copies of their e-cigarette leaflet.
Where did the idea of the Tobacco Dependence Treatment project come from?
Tobacco dependence is the greatest cause of preventable death, ill health and health inequality in our patients. Four of the five biggest killers in our local boroughs are smoking related (cancer, stroke, heart disease and lung disease). At King’s College Hospital NHS Foundation Trust (KCH) alone tobacco dependence accounts for approximately 6,500 admissions per year.
The Ottawa Model, has been found to improve quit rates and result in significant and sustained reductions in mortality, rehospitalisation, and Emergency Department use in sick smokers. An innovative version of the Ottawa Model to provide routine specialist treatment to inpatient smokers commenced at KCH in January 2020.
Can you describe the TDT process to us?
Inpatients identified as current smokers are offered medication and supported by the Tobacco Dependence Specialists to either make a quit attempt or maintain temporary abstinence during their admission, in line with the Trust Smokefree Policy. Patients receive continuing care via scheduled telephone contact over six months with a member of the Tobacco Dependence Team.
What has been the most positive impact for patients/staff?
Staff on these wards received specialist training and ongoing support from the Tobacco Dependence Specialists to develop their skills in treating tobacco dependence. We know that the majority of smokers want to stop smoking, and probably have tried before to quit. The system ensures that our sick patients that smoke receive the routine specialist support they need.
Patients have been very keen to engage with our service and have appreciated our calls. A follow-up call from the hospital Tobacco Dependence Team post-discharge ensures continuity of care and builds on the supportive relationship initiated on the ward by the specialist.
What will the impact of your work be/what are your ambitions for improving outcomes for patients in south east London?
In the first year of operation the team reviewed 81% of identified smokers on selected wards and 14% of patients were smokefree at the 12 week follow up call. This is a significant achievement, given the project that was delivered during a global pandemic. With additional funding support we have recruited more Tobacco Dependence Specialists to support more of our patients that smoke to go smokefree.
How has working across King’s Health Partners (KHP) facilitated your work?
This has been a KHP project from the start, working with our colleagues from Guy’s & St Thomas’ NHS Foundation Trust to share experience and learning. We are also fortunate to have academic support from our colleagues at King’s College London to help drive the project forward.
 *Tobacco Dependence Team at King’s College Hospital NHS Foundation Trust are:
*Tobacco Dependence Team at King’s College Hospital NHS Foundation Trust are:
Arran Woodhouse – Lead Tobacco Dependence Specialist
Sherine Simpson – Tobacco Dependence Co-ordinator
Sandra White – Tobacco Dependence Co-ordinator
Stephanie Duckworth-Porras – Tobacco Dependence Specialist
Andrew Stock – Tobacco Dependence Specialist
Olga Guba – Tobacco Dependence Specialist
Kaya Mahdavieh – Tobacco Dependence Specialist
Geraldine Brown – Tobacco Dependence Specialist